Streptococcus suis causes bacterial meningitis with hearing loss in patients without direct exposure to pigs in a regional pork industry territory
Article information
Abstract
Streptococcus suis (S. suis) is an emerging zoonotic pathogen that causes bacterial meningitis in humans. S. suis is an encapsulated gram-positive facultative anaerobic bacterium and is an important pathogen in pigs. This infectious disease usually manifests in humans as meningitis, endocarditis, septicemia, and arthritis. Most cases originate in Southeast Asia, and human S. suis infections are often reported in countries with a high density of pigs. Meningitis is a common clinical manifestation of S. suis infection. Moreover, hearing loss is a common complication that can be bilateral, profound, and/or permanent. This report presents two cases of bacterial meningitis and hearing loss caused by S. suis in patients without a history of direct exposure to pigs in an intensive pork industry region.
INTRODUCTION
Streptococcus suis (S. suis) is an encapsulated grampositive, facultative anaerobic bacterium [1]. This is a primarily swine pathogen, and S. suis infection in pigs has been reported globally [2]. Since the first human case in Denmark [3], an increasing number of human cases have been reported in many countries, and an outbreak of S. suis infection has occurred in China [4]. Human S. suis infection presents as meningitis, endocarditis, septicemia, and arthritis. Patients with meningitis can develop permanent hearing loss [5]. Thus, this infectious disease is an emerging zoonosis and significant public health threat [1].
Human S. suis infections are often reported in countries that engage in high levels of pig farming [6]. Risk factors for human infection include contact with contaminated pork, consumption of raw pork, slaughtering, butchering carcasses, and processing sick or dead pigs [4]. The pork industry has become one of the main pillars supporting Jeju Island’s economy [7], and human S. suis infection cases have not yet been reported in this region. This report presents two patients with no direct exposure to pork or pigs who developed bacterial meningitis and hearing loss caused by S. suis on Jeju Island with a brief review of the literature.
CASE REPORT
1. Case 1
A 45-year-old fisherman presented with decreased awareness, excessive sweating, prosopagnosia, nausea, and intractable headache for 3 days. The patient had a history of heavy alcohol consumption. On the day of admission, the blood pressure was 140/100 mmHg, pulse rate was 70 beats/min, respiratory rate was 20 breaths/min, and temperature was 37.1°C. Physical examination revealed confusion, emotional incontinence, and neck stiffness. Laboratory results revealed a white blood cell (WBC) count of 22,000/μL (normal range, 4,000−10,000), with 88.7% polymorphonuclear cells, and platelet count of 76,000/μL (normal range, 150,000−450,000). The serum C-reactive protein level was 33.76 mg/dL (normal range, 0.0−0.3), and the erythrocyte sedimentation rate was 90 mm/h (normal range, 0−9). The serum creatinine level was 1.21 mg/dL (normal range, 0.5−0.9). The patient’s cerebrospinal fluid (CSF) was turbid and yellowish with an opening pressure of 35 cmH2O. CSF analysis revealed a WBC count of 5,700/µL (polymorphonuclear cells, 70%), protein concentration of 232 mg/dL, and glucose concentration of 60 mg/dL (serum glucose, 206 mg/dL). After CSF analysis and collection of samples for peripheral blood culture, empirical antibiotic treatment with 2,000 mg ampicillin four times a day, 2,000 mg ceftriaxone twice a day, and 1,000 mg vancomycin three times a day was administered intravenously. Additionally, intravenous dexamethasone (10 mg every 6 hours) was administered to decrease meningeal inflammation and prevent neurologic complications.
Brain magnetic resonance imaging (MRI) showed an abnormally high leptomeningeal signal intensity in both temporo-occipital areas (Fig. 1A). Fluid-attenuated inversion recovery showed a bright signal in both mastoids, noted as bilateral mastoiditis (Fig. 1B). Computed tomography revealed that the source of the bright signal was the bone marrow of an unpneumatized mastoid bone (Fig. 1C, D).

Neuroimaging of patient 1. (A) Brain magnetic resonance imaging showed abnormally high signal intensity of the leptomeninges in both temporo-occipital areas (white arrows). (B) Fluid-attenuated inversion recovery shows a bright signal (arrows) in both mastoids, noted as bilateral mastoiditis. (C, D) Computed tomography showed the source of the bright signal to be the bone marrow of an unpneumatized mastoid bone (white arrows).
The patient’s consciousness and severe headache gradually resolved, and hearing impairment and diplopia developed on the 3rd day of admission. Pure-tone audiometry revealed profound bilateral sensorineural hearing loss.
On the fifth day of admission, blood cultures were negative on an automated VITEK II system (BioMerieux, Durham, NC, USA). Gram-positive cocci were observed in the initial CSF specimen, and the CSF culture results showed S. suis as susceptible to beta-lactams, quinolones, and vancomycin. He had no exposure to raw pork and no history of contact with livestock. After a 2-week course of antibiotic therapy, his symptoms markedly improved, except for hearing loss.
2. Case 2
A 58-year-old man was transferred to our emergency department because of acute confusion. He showed acute abnormal behavior with a history of vomiting for approximately 7 days before admission. On admission, physical examination revealed a Glasgow coma scale score of 12 (E4V3M5), blood pressure of 109/63 mmHg, heart rate of 111 beats/min, respiratory rate of 20 breaths/min, and temperature of 38.3°C. Neurological examination revealed absence of motor laterality or pathological reflex, except for nuchal rigidity. Initial brain MRI revealed no focal pathology, but there was overall mild brain swelling. Laboratory results revealed a WBC count of 6,900/μL (normal range, 4,000−10,000) with 72.7% polymorphonuclear cells and platelet count of 20,000/μL (normal range, 150,000−450,000). The serum C-reactive protein level was 28.62 mg/dL (normal range, 0.0−0.3), and the erythrocyte sedimentation rate was 90 mm/h (normal range, 0−9). The serum creatinine level was 1.3 mg/dL (normal range, 0.5−0.9). Liver function tests revealed an alanine aminotransferase level of 73 IU/L (normal range, 4−44), aspartate aminotransferase level of 78 IU/L (normal range, 8−38), alkaline phosphatase level of 393 U/L (normal range, 104−338), and gamma-glutamyl transpeptidase level of 406 U/L (normal range, 10−71). The procalcitonin level was 2.46 ng/mL (normal range, 0−0.05). The patient’s CSF was yellowish, and the opening pressure was 38 cmH2O. CSF analysis revealed a WBC count of 975/µL (polymorphonuclear cells, 60%), protein concentration of 240 mg/dL, and glucose concentration of 24 mg/dL (serum glucose, 155 mg/dL). After performing CSF analysis and obtaining samples for peripheral blood cultures, empirical antibiotic treatment with ampicillin 2,000 mg four times a day, ceftriaxone 2,000 mg twice a day, and vancomycin 1,000 mg three times a day was administered intravenously. Antibiotic therapy was administered along with intravenous dexamethasone, which was maintained for 5 days.
S. suis, which is susceptible to all antibiotics, was identified on blood culture, and penicillin G was administered at 24 million IU every 24 hours. On the 7th day of admission, follow-up lumbar puncture showed that the CSF was clear and had 100 leukocytes/µL (polymorphonuclear cells, 1%). The protein concentration was 48 mg/dL, and the glucose concentration was 62 mg/dL (serum glucose, 140 mg/dL).
On the 8th day of admission, pure tone audiometry revealed bilateral sensorineural hearing loss. Brain MRI revealed nonspecific gliosis and leukoaraiosis. On day 23 of admission, the patient was discharged, having completely recovered. He denied any pig or pork exposure during the past several months. His sensory neuronal hearing loss did not improve after 6 months.
DISCUSSION
We described the clinical characteristics and microbiological results of two cases of human S. suis infection on Jeju Island, South Korea (Supplementary Fig. 1). The two patients had no history of direct pig contact or raw pork consumption. Jeju black pigs are famous in the South [8], and this region has specialized and focused on the pig industry. Most pigs are bred in clean, modern environments. Nevertheless, more than 500,000 pigs are raised in Jeju Island (1,846 km2 of area), and unintentional exposure to contaminated pork is feasible [7]. Additionally, acute bacterial meningitis caused by S. suis might be a public health concern as a potentially severe zoonotic infectious disease that contaminates the Jeju pork industry. Our study identified S. suis as one of the recognized causes of acute bacterial meningitis on Jeju Island, South Korea.
S. suis is an important etiology of bacterial meningitis in non-immunocompromised and immunocompromised patients, regardless of their pig contact status in South Asia [1]. The clinical manifestations of meningitis caused by S. suis are similar to that of patients with bacterial meningitis caused by Neisseria meningitidis and Streptococcus pneumoniae. The most distinctive feature of S. suis meningitis is progressive hearing loss, resulting in bilateral deafness in most patients [9]. The mechanism of hearing loss in S. suis meningitis is not yet well understood. Animal studies have suggested that the cochlea is directly involved during the spread of S. suis infection.
Phylogenetic analysis revealed that the S. suis strains isolated in cases 1 and 2 were similar to strains previously isolated in the Republic of Korea, China, Japan, and Taiwan (Fig. 2) [10]. S. suis can be transmitted through the nasal or oral cavity and colonize the palatine tonsils [6]. Most human infections seem related to slaughtering, butchering carcasses, and processing of sick or dead pigs [4]. However, occupational exposure to contaminated pork is not present in all cases of S. suis infection. Since Jeju Island is a wellknown pig industry territory and pork consumption is high, it is reasonable that the patients in these cases were unknowingly exposed and infected. Thus, even if there is no history of direct exposure to pigs or pig byproducts, bacterial meningitis can be caused by unpredictable exposure to S. suis on Jeju Island, and neurologic complications, including hearing loss, can occur despite proper medical management.
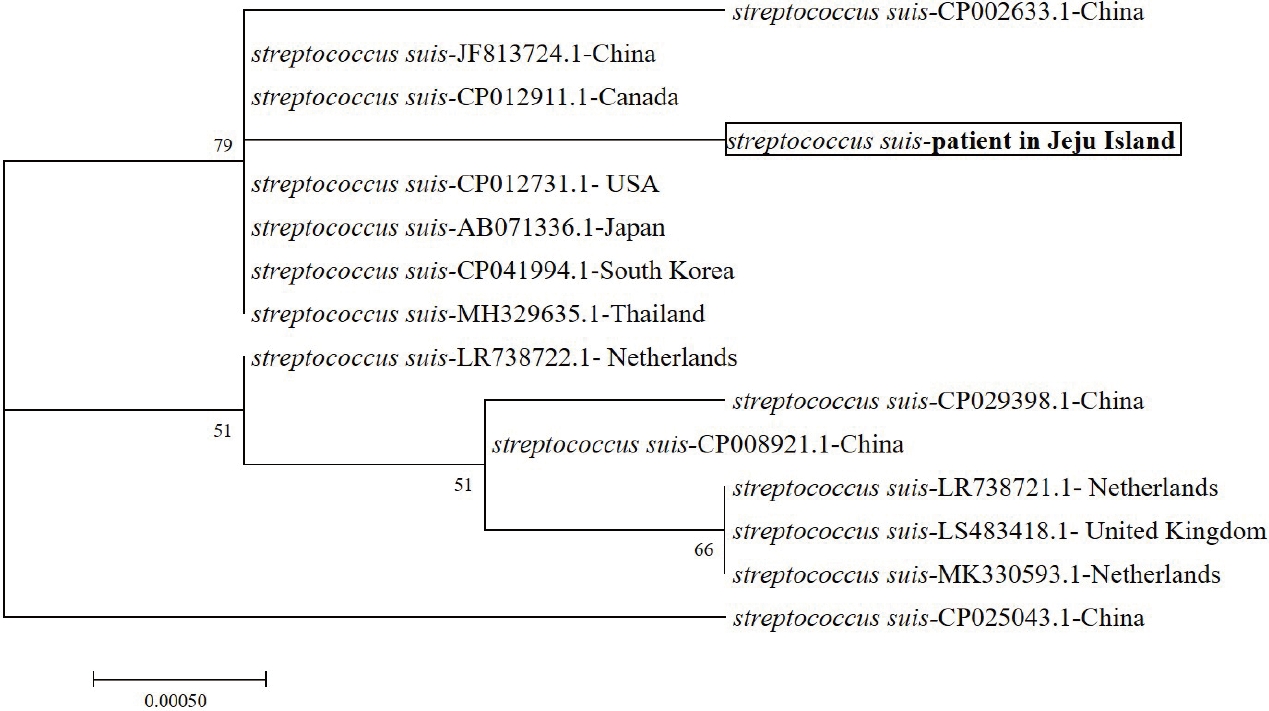
Molecular phylogenetic tree constructed by the neighbor-joining method using the 16S rRNA gene sequences of patient’s Streptococcus suis isolate and various Streptococcus species. The reference sequences were from the type strains of the species, and the accession numbers are given in parentheses. All names and accession numbers are given as cited in the GenBank database.
Recognition of the possibility of deafness in patients diagnosed with S. suis meningitis without a direct pig exposure history is essential. Early diagnosis and treatment are crucial for reducing symptomatic sequelae, which would critically impact the clinical outcome and quality of life after aggressive medical treatment. Additional studies are necessary to elucidate the routes for infection of the general population by S. suis and bacterial meningitis in the pork industry in Jeju Island.
Supplementary Material
Supplementary Figure 1.
Geographic location of Jeju Island in the Republic of Korea. The black box indicates the region of Jeju Island. Jeju Island is the largest island in the Korean Peninsula. It has a subtropical climate, according to Trewartha’s subtropical climate definition, and a population of 690,000, approximately 15% of whom are farmers. Generally, many domestic and wild animals are present in ordinary fields or coastal areas of this island.
Acknowledgements
This work was supported by a research grant from Jeju National University Hospital in 2019.