Body mass index and massive hemorrhage after cesarean section in patients with placenta previa
Article information
Abstract
This study was undertaken to assess the potential of body mass index (BMI) as a risk factor for massive hemorrhage (MH) after cesarean section (CS) in patients with placenta previa. We retrospectively reviewed the medical records of patients who underwent CS for placenta previa between January 2010 and December 2018. MH was defined as an estimated blood loss ≥2,000 mL during surgery. Clinical characteristics, including BMI, were compared between the groups with and without MH. Subsequently, multivariable logistic regression analysis was conducted to identify the independent risk factors for MH. A total of 189 patients were included in this study. MH was observed in 28 patients (14.8%). According to the multivariable logistic regression analysis results, the risk factors independently associated with MH were BMI at delivery (adjusted odds ratio [aOR], 1.19; 95% confidence interval [CI], 1.04-1.35; P=0.012), placenta accreta (aOR, 24.55; 95% CI, 2.75-219.02; P=0.004), and total previa degree (aOR, 9.86; 95% CI, 2.71-35.96; P=0.001). The study findings showed that maternal obesity, namely a higher BMI at delivery, was an independent risk factor for MH after CS in patients with placenta previa. Close attention should be paid to the potential risk of hemorrhage associated with maternal obesity as well as the well-known risk factors of placenta accreta and total previa degree.
INTRODUCTION
Placenta previa (PP), an obstetric condition in which the placenta abnormally implants at the bottom of the uterus, has an overall global prevalence rate of 4 per 1,000 births [1]. It is well known that PP is associated with massive hemorrhage (MH) after cesarean section (CS), which could lead to maternal morbidity and mortality. Therefore, it is important to identify the potential risk factors to enable proper planning and management of obstetric anesthesia.
While research findings on the commonly reported risk factors for postpartum hemorrhage in cases of PP, such as maternal age, gestational age, previous CS, previous abortion, total previa degree, anterior placental position, and placenta accreta, have been inconsistent [2-5], maternal obesity has been linked to several important adverse obstetric outcomes, including postpartum hemorrhage [6-8]. However, few studies have investigated the association between maternal obesity and postpartum hemorrhage, especially in cases of PP, and the association remains obscure. This study aimed to investigate the potential of body mass index (BMI) as a risk factor for MH after CS in patients with PP.
METHODS
This study was approved by Institutional Review Board (IRB) of Jeju National University Hospital (IRB No. 019-04-001). We retrospectively reviewed the medical records of patients with PP who underwent CS at Jeju National University Hospital between January 2010 and December 2018.
Twin pregnancies were excluded from the analysis. Furthermore, since most of the CSs were performed by two obstetric surgeons, patients who underwent CS performed by other surgeons were excluded to reduce surgical bias. Additionally, patients who underwent surgical procedures other than low transverse uterine incision were excluded for the same reason.
MH was defined as an estimated blood loss ≥2,000 mL during surgery. The variables collected included maternal age, BMI, American Society of Anesthesiologists class, gestational age, previous abortion, previous vaginal delivery, previous CS, previous uterine surgery except for CS, presence of conditions, such as uterine myoma; gestational diabetes; gestational hypertension or preeclampsia; antenatal hemorrhage; and placenta accrete, antenatal use of tocolytics, emergent CS, total previa degree, and anterior placental position.
To compare the variables between the groups with and without MH, the Chi-square test or Fisher’s exact test was performed for categorical data, and the Mann-Whitney test was performed for numerical data. Thereafter, variables with a P-value <0.1 in the univariable analysis were chosen for multivariable logistic regression analysis. The data were analyzed using IBM SPSS (version 20.0; IBM Co., Armonk, NY, USA). The statistical significance was set at P<0.05.
RESULTS
In total, 219 patients underwent CS for PP during the study period. Eighteen patients with twin gestations were excluded from analysis. Nine patients in whom CS was performed by other surgeons and three patients who underwent surgical procedures other than low transverse uterine incision were also excluded. A total of 189 patients were analyzed (Fig. 1).
MH was observed in 28 out of 189 patients (14.8%). The median estimated blood loss was 1,000 mL in the non-MH group and 2,800 mL in the MH group. There was no statistically significant difference in the incidence of MH between the two surgeons. Patients with MH more often received general anesthesia than those without MH. However, we did not include the type of anesthesia in the multivariable analysis, as explained later.
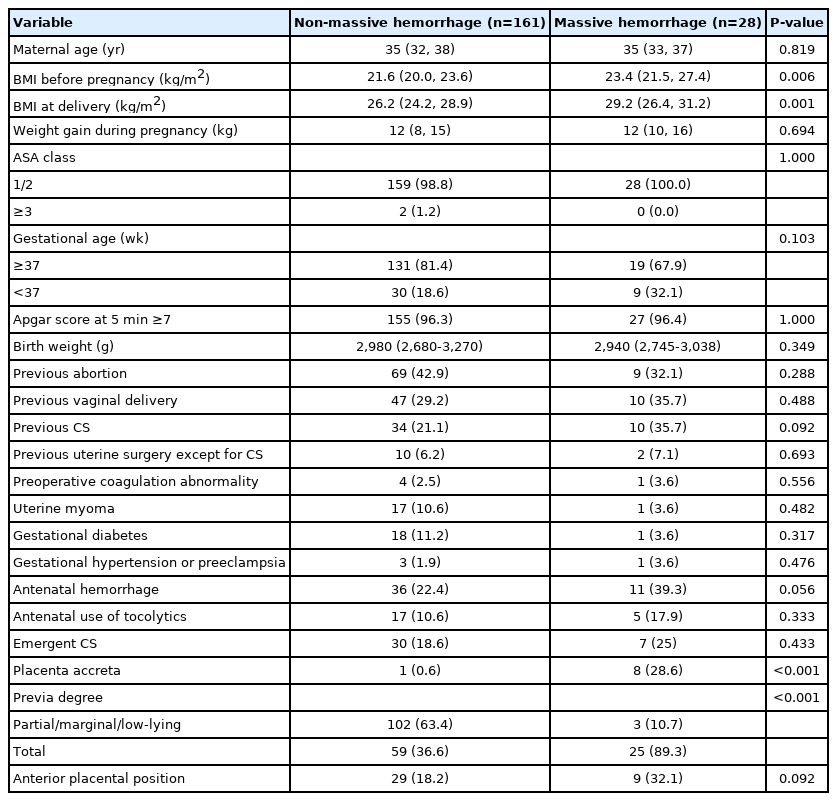
Patients with MH received higher units of packed red blood cells within 24 hours after delivery. The preoperative hemoglobin level was not different between the two groups; however, the predischarge hemoglobin level was l]ower in the MH group even though the patients in this group had received more blood transfusions. Four patients with MH developed pneumonia, cardiomyopathy, or ischemic liver injury after the operation; however, maternal mortality was not observed in either group (Table 1).
In the univariable analysis, patients with MH had higher BMIs both before pregnancy and at deliver y. Weight gain during pregnancy did not differ between the two groups. The variables considered in the multivariable analysis included BMI at delivery, previous CS, antenatal hemorrhage, placenta accreta, total previa degree, and anterior placental position (Table 2).
The results of the multivariable logistic regression analysis indicated that the risk factors independently associated with MH were BMI at delivery, placenta accreta, and total degree of previa (Table 3).
DISCUSSION
Obstetric hemorrhage accounts for more than 25% of maternal deaths worldwide and is one of the three leading causes of maternal death, along with hypertensive disorders and embolisms. Among the types of obstetric hemorrhage, postpartum hemorrhage is the most common cause of maternal mortality. Park and Kwon [9] reported that postpartum hemorrhage was the second most common cause of maternal mortality in Korea from 2009 to 2014. This highlighted the need for eff icient management approaches, including risk factor identification.
PP is a significant obstetric complication associated with MH. In this study, MH was observed in 28 out of 189 patients with PP (14.8%). This is consistent with the results of previous studies in which 10.2-20.5% of the patients with PP experienced MH during CS [2,3]. When MH develops during the anesthetic management of patients with PP, thorough preparation for blood transfusion and close monitoring are required. Therefore, in this study, we aimed to determine the causes of MH during CS in patients with PP.
In this study, we demonstrated that the risk factors independently associated with MH after CS in patients with PP were higher BMI at delivery, placenta accreta, and total degree of previa. Other risk factors, such as previous CS, antenatal hemorrhage, and anterior placental position, were shown to be correlated with MH in the univariable analysis; however, the association was lost in the multivariable analysis due to the presence of confounding factors.
Including a difference in the degree, the number of obese women of childbearing age in developed countries has continued to increase over the past decades. Accordingly, several population-based studies have investigated the relationship between increased mater nal obesity and postpartum hemorrhage. However, despite several studies, the relationship between maternal obesity and postpartum hemorrhage remains controversial. Some studies have reported that a higher BMI was associated with a higher incidence of postpar tum hemor rhage [6,8], while others have reported that a higher BMI was not associated with post par tum hemor rhage [10 -12] and that it even reduced postpartum hemorrhage [7].
These conflicting results may have been due to the use of different definitions of postpartum hemorrhage, lack of control over the mode of delivery, or uniformity in the timing of the body weight measurements used to calculate the maternal BMI. The definition of postpartum hemorrhage differed from study to study and included bleeding volume ranging from ≥500 mL to ≥1,000 mL [6,8]. The definition of MH also varied, including conditions that required hysterectomy or surgical interventions [12], hemorrhages requiring transfusion [7,11], and hemorrhages greater than 2,500 mL [2,3]. Additionally, several types of body weight were used, such as pre-pregnancy weight 8) or weight measured at the first obstetric visit [6,7,10].
We focused on identifying the independent risk factors involved in the occurrence of an MH event ≥2,000 mL during CS in patients with PP. Clinically, if bleeding ≥2,000 mL occurs, blood transfusions, including several units of packed red blood cells, close monitoring, and high-level anesthetic management are required. In this study, the median number of packed red blood cells transfused within 24 hours after delivery was zero in the non-MH group and six in the MH group.
In our study, we compared BMI before pregnancy, BMI at delivery, and weight gain during pregnancy between the two groups. There was no difference in the weight gained during pregnancy between the two groups. However, patients with MH had higher BMIs both before pregnancy and at delivery than those without MH. From the results of the multivariable analysis, a higher BMI was found to be independently associated with an increased risk of MH.
Maternal obesity is linked to several important adverse obstetric outcomes, including postpartum hemorrhage, and is associated with various obstetric complications, such as an increased rate of CS, preeclampsia, and the use of tocolytics, all of which may contribute to the increased risk of postpartum hemorrhage [6-8]. However, since few studies have investigated the association between maternal obesity and MH after CS, especially in cases of PP, further studies are needed to clarify this.
Placenta accreta is a well-known risk factor of MH in patients with PP. In this study, women with placenta accreta showed a nearly 27-fold increase in the odds of developing MH. Placenta accreta is thought to be due to the absence or deficiency of Nitabuch’s layer or the spongiosum layer of the decidua. A history of CS or other uterine surgeries can increase the risk of both PP and placenta accreta. Sonographic findings, such as the existence of an irregularly shaped placenta lacunae, thinning of the myometrium overlying the placenta, lack of a clear zone, and increased vascularity of the uterine serosa, have been suggested as predictive factors for placenta accreta [13,14]. Women with suspected placenta accreta should be examined and managed carefully.
The degree of previa is another well-known risk factor for postpartum hemorrhage. Several studies have reported that the total previa degree was related to a higher frequency of postpartum hemorrhage, higher requirement for postpartum blood transfusions, and hysterectomy [5,11]. Similarly, in the present study, the risk of MH was higher in patients with total PP than in patients with partial, marginal, or low-lying PP.
With respect to the risk factors identified in this study, BMI at delivery was a determining parameter, whereas placenta accreta and total previa degree could be predicted by sonographic examination. The findings of this study indicated that it would be helpful to preoperatively check BMI at delivery, placenta accreta, and total previa degree to prepare personnel, monitoring equipment, and blood components accordingly.
This study had several limitations. First, in this study, MH was defined according to the estimated blood loss in the medical records. We determined the estimated blood loss based on the blood collected in the surgical field, suction bottle, and surgical gauze. Clinical findings, such as cardiovascular changes and the amount of fluid or blood products administered, were also considered. However, the differences between the clinical estimates and actual blood loss have been demonstrated in several studies, and the most common error is underestimation [15-17]. Therefore, it should be considered that more patients may experience MH than observed from the results of this study.
Another limitation was that the incidence of general anesthesia use or conversion to general anesthesia after spinal or epidural anesthesia occur red more often in patients with MH. In Jeju National University Hospital, CS is routinely performed under spinal or epidural anesthesia. General anesthesia is administered only in a few exceptional cases where a large amount of bleeding is expected by the obstetric surgeon or anesthesiologist or when the patient has coagulation abnormalities. Therefore, although general anesthesia is considered a risk factor for postpartum hemorrhage, the anesthetic method was not analyzed in this study. Finally, with regard to race, which was also considered a risk factor for postpartum hemorrhage, the participants in this study were all Asians. Further research is needed to determine whether race is a risk factor.
In conclusion, the study findings showed that maternal obesity, namely a higher BMI at delivery, was an independent risk factor for MH after CS in patients with PP. Close attention should be paid to the potential risk of hemorrhage associated with maternal obesity as well as the well-known risk factors of placenta accreta and total previa degree.