Unilateral hypoglossal nerve palsy after mild COVID-19: a case report
Article information
Abstract
Post-acute coronavirus disease (COVID-19) syndrome is defined as persistent symptoms or delayed complications after COVID-19. Several cases of cranial nerve invasion related to COVID-19 have been reported. However, to our knowledge, no cases of solitary unilateral hypoglossal nerve paralysis after mild COVID-19 without intubation have been reported to date. Herein, we report the case of a 64-year-old man with unilateral hypoglossal nerve palsy as a complication of COVID-19. He complained of dysarthria and tongue discomfort 2 weeks after COVID-19 onset. Brain and neck computed tomography, magnetic resonance imaging, ultrasonography, and blood tests ruled out other possible causes. The patient’s nerve palsy was rapidly diagnosed and improved with early rehabilitation. Understanding of the pathology of COVID-19 is still limited. Physicians should focus on patients’ symptoms and their relationship to COVID-19, and investigate complications immediately. This case highlights the importance of early detection and rehabilitation of post-acute COVID-19 syndrome.
INTRODUCTION
Coronavirus disease (COVID-19), a pandemic respiratory infectious disease caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), which was first reported in Wuhan, China, in 2019. Several vaccines and medications have been developed, and the pandemic is decreasing. However, post-acute COVID-19 syndrome, persistent symptoms, and delayed complications after COVID-19 are now a problem [1]. Although most complications involve the respiratory tract, several cases of neurological complications related to SARS-CoV-2 have often been reported [2-5].
The hypoglossal nerve, also known as the cranial nerve (CN) XII, is a motor nerve that innervates the tongue muscles. It originates from the hypoglossal nucleus in the medulla, traverses the hypoglossal canal and the carotid bifurcation, and innervates the tongue. Hypoglossal nerve palsy (HNP) is a rare condition characterized by dysphagia, dysarthria, and tongue discomfort. Owing to its various etiologies, other diseases must be ruled out through imaging studies and meticulous clinical history taking [6-8].
Inflammation is the reported cause of HNP in 7.3% of cases [7]. Viral infections can also cause HNP. Several cases of multiple CN damage, including hypoglossal nerve, have been reported in critically ill patients with COVID-19 [2,5]. Only one COVID-19-associated case of isolated hypoglossal nerve damage has previously been reported; however, the possibility of HNP due to intubation and intensive care could not be ruled out [9]. Herein, we reported a case of a patient whose hypoglossal nerve was paralyzed after mild COVID-19 without intubation or a history of intensive care.
CASE REPORT
A 64-year-old man taking medications for diabetes and hyperlipidemia complained of coughing and sputum production in April 2022. He tested positive for SARS-CoV-2 on polymerase chain reaction testing. He had a sore throat and throat discomfort without thirst, dyspnea, or fever. He received symptomatic treatment with nonsteroidal anti-inf lammatory drugs at home and recovered from COVID-19 without specific complications. Two weeks after being released from quarantine, he complained of dysarthria and tongue discomfort. Brain computed tomography (CT) and magnetic resonance imaging (MRI) were performed in neurology department to investigate possible cerebrovascular disease. Brain MRI revealed non-specific findings in the vessels and brain parenchyma but T2-weighted imaging revealed a diffuse high-signal change on the left side of the tongue (Fig. 1). The patient was subsequently transferred to the otorhinolaryngology department of a tertiary hospital for evaluation of the tongue mass. Physical examination revealed atrophy and movement limitation on the left side of the tongue (Fig. 2), but no palpable tongue mass. Visual, olfactory, and auditory functions, facial movements, gag reflex, shoulder movement, and bilateral vocal cord mobility were normal on cranial nerve examination. The sensory and motor functions of his arms and legs were intact. The patient did not show any signs of cervical spinal nerve dysfunction, such as weakness of the geniohyoid, omohyoid, or sternohyoid muscles. Limited tongue movement was the only abnormality, and the atrophy and deviations were typical of HNP. Therefore, we suspected unilateral HNP and performed neck CT, MRI, ultrasonography, and blood tests to determine the cause. No abnormalities that could cause HNP were identified, and the only abnormalities identified were signal changes of both the intrinsic and extrinsic muscles of the left side of the tongue. It was not possible to localize the exact point of damage to the hypoglossal nerve. However, based on visible muscle atrophy and the inability to protrude the tongue, it appears that there was dysfunction in both the intrinsic and extrinsic tongue muscles. He was diagnosed with unilateral HNP as a complication of COVID-19. He was taught rehabilitation exercises that could be easily performed at home. At the 1-month follow-up visit, most tongue movements and symptoms had improved, but there was a slight difference in the volume of the two sides of the tongue. No objective data are available on the functional improvements because the patient declined objective tests and further follow-up.
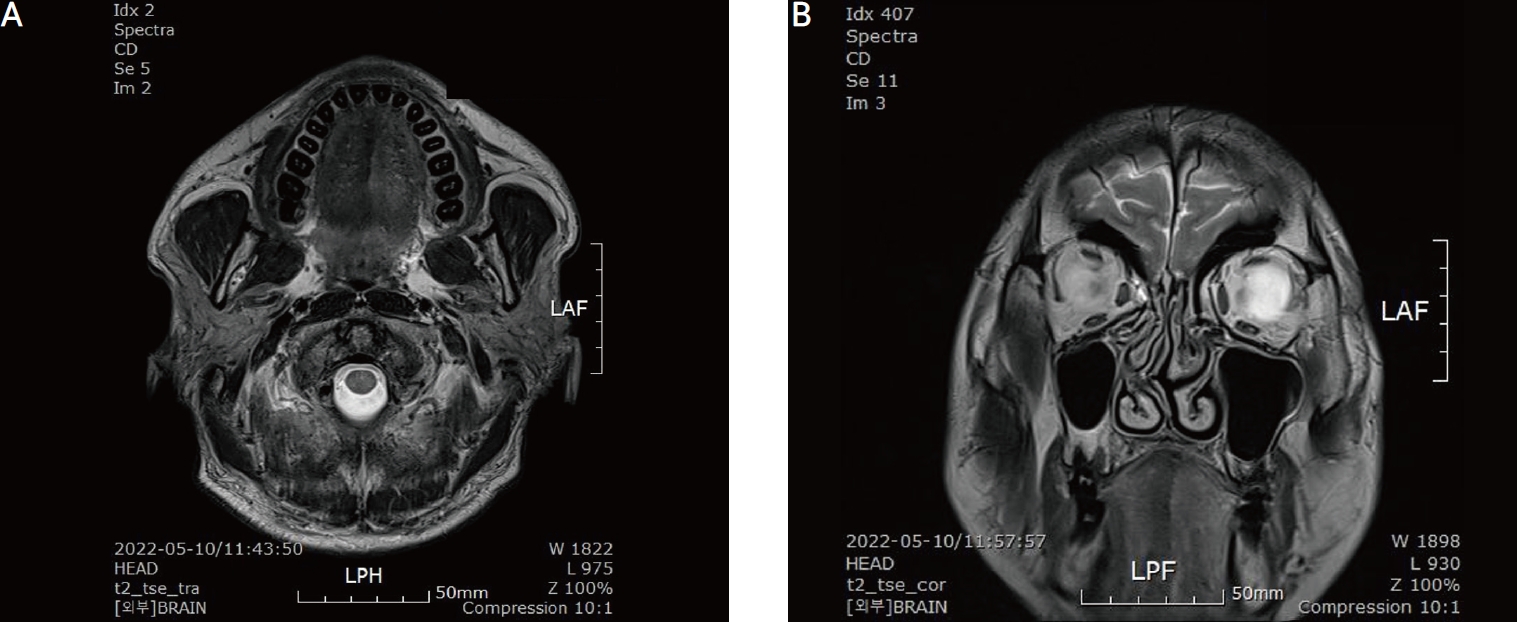
Brain magnetic resonance imaging (MRI) showing a diffuse high-signal change at the left hemi-tongue with no abnormalities in the vessels and brain parenchyma. T2-weighted MRI axial view (A), T2-weighted MRI coronal view (B).
DISCUSSION
Several post-acute COVID-19 syndromes affect the CN. This can occur in every CN, from I to XII. Furthermore, it can involve multiple nerves [2-5]. In our case, only CN XII was paralyzed. To evaluate systemic neurological function and infection, we recommend nerve conduction studies, electromyography, and cerebrospinal fluid testing. However, the patient refused the tests because he experienced only lingual discomfort, which was tolerable. We explained that additional tests would be necessary if he developed other neurological symptoms or if his symptoms did not improve. In patients with post-acute COVID-19 syndromes involving the CN, accompanying neurological signs must be assessed and the need for additional examinations, such as nerve conduction studies, electromyography, and cerebrospinal fluid tests, must be explained.
The exact mechanism of nerve injury after SARS-CoV-2 infection has not yet been elucidated. In a recent clinical study, Yavarpour-Bali and Ghasemi-Kasman [10] explained two mechanisms whereby SARS-CoV-2 can access the human nervous system. First, SARS-CoV-2 can directly invade the nerve through angiotensin-converting enzyme 2 receptors. Viruses in the blood can invade the blood-brain barrier and blood-cerebrospinal fluid barrier. Second, SARS-CoV-2 can invade the nerve through retrograde and anterograde axonal transport along peripheral nerves. In this case, the patient’s symptoms were mild and were not considered indicative of viremia. Therefore, the axonal transport mechanism through peripheral nerves is a more likely mechanism in this case. Further research is required to identify the exact mechanisms of neuroinvasion in patients with COVID-19.
Dysarthria is a primary symptom of stroke. In patients with dysarthria, immediate evaluation of brain images is important to assess whether cerebrovascular disease is present and can affect the prognosis. Although dysarthria is generally caused by problems in the central nervous system, it can be caused by peripheral nervous system problems such as HNP. When conducting a diagnostic evaluation in patients with dysarthria, physicians should not fail to open the patient’s mouth and examine the tongue and perform a cranial nerve evaluation, despite the urgency.
To our knowledge, this is the first reported case of HNP as a complication of mild COVID-19 without intubation. Understanding of the pathology of COVID-19 is still limited and its symptoms can involve any system. As the COVID-19 pandemic is ongoing, physicians should focus on each patient’s symptoms and ask about their history of COVID-19. This case highlights the importance of early detection and rehabilitation for post-acute COVID-19 syndrome.
Acknowledgements
The authors declare no conflicts of interest in this article.

