Consideration of fractionation or field size prior to radiation therapy in patients with breast cancer and psoriasis: a case report
Article information
Abstract
We present three cases of patients with breast cancer and psoriasis who received radiotherapy following breast-conserving surgery. One patient developed an extensive flare-up of psoriasis during chemotherapy. After discontinuing chemotherapy, she received conventional radiotherapy to the ipsilateral whole breast, axillary, and supraclavicular lymph nodes with 50.4 Gy in 28 fractions and boosted with 10 Gy in five fractions to the tumor bed. Two patients received hypofractionated whole-breast radiotherapy at a total dose of 40.05–42.4 Gy in 15–16 fractions. In all three cases, there was no flare-up of psoriatic events at least 6 months after the completion of radiotherapy. We hypothesized that there is a close relationship between psoriatic events and the extent of trauma rather than the daily dose of the fraction. Therefore, we confirmed that the effect of radiotherapy on psoriatic events is minimal if the radiation field size does not exceed that of the whole breast.
INTRODUCTION
Psoriasis is characterized by chronic and recurrent skin lesions and has a wide spectrum of clinical courses [1]. Common symptoms include red, inflamed skin, and scaly plaques [2]. More severe cases can influence both, emotional and social aspects of a patient’s life [3]. Several reports have described patients with breast cancer who developed erythrodermic psoriasis following radiotherapy, which is mainly attributed to skin trauma due to surgery or radiotherapy.
Considering the rising incidence of breast cancer, radiotherapy should be reconsidered in patients with psoriasis, and if unavoidable, an attempt to spare the involved skin should be performed. It was previously confirmed that using a daily radiotherapy dose ≤2.0 Gy did not exacerbate or cause the development of new psoriatic lesions [4]. Therefore, it is important to understand the risk of psoriasis in patients with hypofractionated radiotherapy or in large fields, including axillary lymph nodes.
To date, there are limited case reports regarding the incidence or exacerbation of psoriatic flare-ups in the irradiation field following whole-breast irradiation [5]. Therefore, we aimed to assess the effect of radiotherapy as a source of skin trauma-triggering events on psoriasis in patients with breast cancer.
CASE REPORT
1. Case 1
A 38-year-old woman with a history of psoriasis, first diagnosed in her 20s was diagnosed with invasive ductal carcinoma of the right breast. The patient underwent breast-conserving surgery with lymph node dissection in August 2019. Pathologically, four of the 20 axillary nodes were involved in the carcinoma, and the tumor stage was determined to be pT2 (2.7 cm) N2 (4/20) M0. Adjuvant chemotherapy was administered. Initially, she received four cycles of doxyrubicin (Adriamycin)-cyclophosphamide, followed by paclitaxel (Taxol). The patient’s psoriasis had remained inactive for more than 7 years. After one cycle of Taxol chemotherapy, she experienced an extensive flare-up involving the scalp, abdomen, back, chest, flanks, buttocks, and both extremities (Fig. 1). Topical corticosteroids were administered after examination by a dermatologist. Considering the existing psoriasis, a radiation oncologist decided to treat the patient with standard fractionated irradiation rather than hypofractionated irradiation. In March 2020, she started radiotherapy of 50.4 Gy in 28 fractions with 6-MV photon beams to the right whole breast, axillary, and supraclavicular lymph nodes and then boosted with 10 Gy in five fractions to the tumor bed. Tamoxifen had also been administered since April 2020. During radiation treatment, mild erythema and hyperpigmentation developed in the radiation field, but there was no psoriatic flare inside or disease progression outside the radiation field. The patient completed radiation therapy in May 2020 without stopping treatment. A recent follow-up examination revealed that her psoriasis had returned to an inactive state in June 2021.
2. Case 2
In April 2020, a 50-year-old patient with a history of severe psoriasis vulgaris involving the scalp, face, abdomen, chest, back, and both extremities presented to our institution. Initially, she received 24 cycles of ultraviolet (UV) therapy, followed by cyclosporine administration for 12 weeks. However, owing to the side effects of UV and cyclosporine, we changed her regimen to guselkumab, which improved her psoriasis. In December 2020, the patient underwent wide excision of the right breast and was diagnosed with ductal carcinoma in situ. The tumor size was 0.3×0.3 cm, and the nuclear grade was low. No additional surgical resection such as axillary node dissection was performed. Tamoxifen was administered one month later. Simultaneously, radiotherapy to the whole breast at a dose of 40.05 Gy in 15 fractions without tumor bed boost irradiation was started. She completed hypofractionated radiotherapy and experienced mild erythema within the radiation field. After radiation therapy, her psoriasis was stabilized by subcutaneous injections of 100 mg guselkumab once a day.
3. Case 3
A 75-year-old woman underwent breast-conserving surgery with lymph node resection for metaplastic carcinoma of the left breast in November 2020. The patient underwent simultaneous total thyroidectomy and central neck dissection for bilateral papillary thyroid cancer. The tumor stage for breast cancer was determined to be pT1 (1.9 cm) N0 (0/5), and adjuvant chemotherapy was administered 1 month later. Considering the patient’s history of psoriasis, early stage of cancer, and advanced age, chemotherapy was discontinued after three cycles of cyclophosphamide/methotrexate/fluorouracil. However, psoriatic lesions improved after chemotherapy. In March 2021, the patient started radiotherapy with hypofractionated radiation to the right whole breast at 42.4 Gy in 16 fractions and boosted with 10 Gy in five fractions to the tumor bed. Anastrozole had also been administered since the initiation of radiotherapy. During a month of radiation treatment, the patient’s psoriasis was stable. She experienced mild erythema of the left breast and itching around the lower back and buttocks (Fig. 2). In August 2021, the patient received radioiodine therapy for thyroid cancer without a psoriatic flare within the radiation field.

Psoriasis was stable during radiation treatment. The patient experienced mild erythema and itching around the lower back and buttock. (A) Flare-up lesion on the arm before radiation treatment, (B) excoriation around the lower back after completion of radiation treatment.
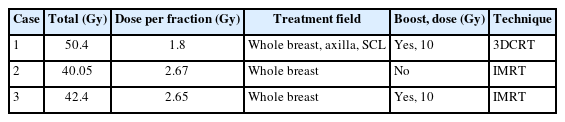
Detailed information regarding the clinical characteristics and radiation treatment profiles of the three patients are presented in Tables 1, 2.
DISCUSSION
The prevalence of psoriasis is estimated to be between 2–3% in the general population, but is 17% higher in patients with breast cancer than that in matched reference individuals [2]. The Koebner phenomenon, first described in 1976, refers to the development of psoriasiform lesions on the skin of patients with psoriasis after cutaneous trauma [6]. Skin trauma, including burns, scratches, and cuts, has been reported as a triggering factor in 43–76% of incident psoriasis cases [7]. The increased risk of psoriasis after breast cancer treatment is clinically plausible, as radiation treatment after surgical resection can cause dermatological side effects.
Radiotherapy plays an important role in managing breast cancer and provides good local control and long-term survival [8]. Radiotherapy to the whole breast with or without a tumor bed boost is needed in cases of breast-conserving surgery; and to the chest wall in cases of mastectomy for tumors >5 cm. Particularly, if lymph nodes are involved, the axillary, supraclavicular, and internal mammary lymph nodal chains should be included, which results in an increased field size compared with whole-breast radiotherapy. According to the National Comprehensive Cancer Network Guidelines, many institutions currently prefer hypofractionated radiotherapy to conventional radiotherapy, in which the whole breast receives a dose of 45-50.4 Gy in 25-28 fractions or 40-42.5 Gy in 15-16 fractions. Previous case reports have revealed that radiation treatment following surgical resection of breast tumors is associated with the Koebner phenomenon. Nevertheless, it is unadvisable to omit radiation therapy in patients with breast cancer with a history of psoriasis.
Ben-Yosef et al. [4] evaluated six patients who received a conventional daily radiation therapy dose ≤2 Gy, assuming that it explains the finding of the Koebner phenomenon. They hypothesized that the daily dose to the skin is a key factor in the development of Koebner phenomenon. Several studies have reported a radiation-induced Koebner phenomenon following radiotherapy in patients with psoriasis who received whole-breast radiotherapy at 50 Gy (2 Gy per fraction) after breast-conserving surgery or postmastectomy radiotherapy to the chest wall at 46 Gy (2.3 Gy per fraction) [9]. Wu et al. [10] described an instance of a skin flare in a 62-year-old woman with a history of active psoriasis who received sequential bilateral hypofractionated whole-breast radiotherapy. However, little is known about the association between dose per fraction or field size and the Koebner phenomenon.
In this report, we included patients with breast cancer with a history of active psoriasis who received radiation therapy following breast-conserving surgery. Two patients received hypofractionated whole-breast radiotherapy with a daily dose of 2.65 or 2.67 Gy. One patient received conventional daily dose radiotherapy for the entire breast and regional lymph nodes. Radiotherapy was performed in patients with breast cancer without severe skin damage. No flare-up of psoriatic lesions was observed in any of the patients, even in cases with a relatively high dose per fraction. Thus, we hypothesized that there is a close relationship between psoriatic events and the extent of trauma, rather than the daily dose of the fraction. This assumption is supported by the findings of a previous report demonstrating that sequential bilateral whole-breast radiotherapy resulted in the Koebner phenomenon.
As a limitation, all three patients underwent breast-conserving surgery, and the conventional daily dose was used for patients who received radiotherapy to the regional lymph nodes in this study. Therefore, it is difficult to conclude whether hypofractionated radiotherapy is safe for patients with psoriasis. Psoriatic events during radiotherapy are closely associated with trauma. If we assume that the extent of trauma is directly proportional to the risk of psoriatic events, it is necessary to pay attention to the use of hypofractionated radiotherapy for patients with mastectomy having a wider range of surgical resection than breast-conserving surgery.
CONCLUSION
This study reported no flare-up of psoriasis in patients with breast cancer following conventional or hypofractionated accelerated radiotherapy. We confirmed that the effect of radiotherapy on psoriatic events was minimal if the radiation field size did not exceed that of the whole breast. Further investigation regarding the skin trauma-triggering factors of radiotherapy, including daily fraction dose and field size, is required.
Acknowledgements
This work was supported by a research grant from Jeju National University Hospital in 2021.